When my babies were born prematurely, we were immediately thrust into a new world with which we were very unfamiliar and unprepared: the NICU. I had an emergency c-section on a Saturday evening and our twins, a boy and a girl, were whisked away to the NICU after a brief meet and greet alongside my head while I was strapped to the operating table. As soon as the babies were taken to the NICU, I instructed my husband and my mom to go with them. My dad unfortunately had a cold at the time, and wasn’t permitted in the NICU. Armed with a mask, he was able to stay with me in the recovery room. It wasn’t until a few hours later, after my spinal anesthesia wore off and I regained feeling in my legs, that I was able to visit the twins in the NICU.
My husband wheeled me down to the NICU in my wheelchair. We stopped at the double doors and he called in for someone to allow us entry. As soon as we entered into the unit, I noticed large frames lining the walls, containing beautiful collages and photos of fragile-looking babies hooked up to machines next to photos of solid and healthy looking toddlers. These were the NICU graduates.
Hubby showed me the ropes and instructed me to scrub my hands at the hand washing station and to put on a yellow gown before we could proceed any further inside. Machines beeped incessantly and there was an eerily somber mood inside. I felt as though I was in a library. Although it wasn’t posted anywhere, it seemed to be the assumed etiquette that you couldn’t talk loudly while inside the NICU. Curtains were drawn around surrounding isolettes, providing privacy for families who were visiting with their babies. Because it was late at night, it was fairly empty and it seemed that most of the babies were sleeping. The lights were dim over each baby, but the bright fluorescent lights over the nurse’s station illuminated a good portion of the unit.
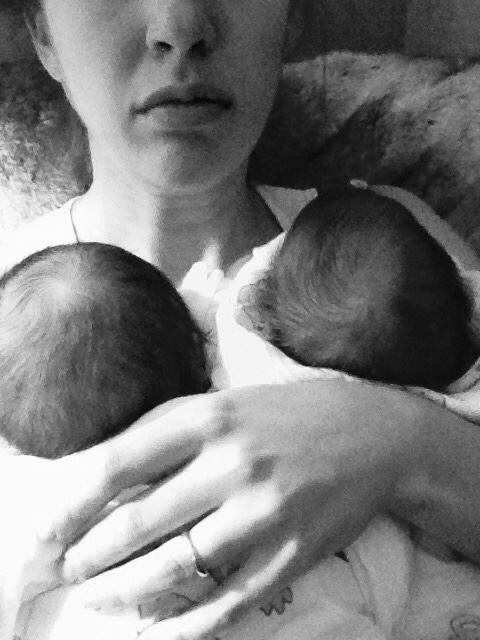
Hubby wheeled me over to the area immediately in front of the nurse’s station where our daughter was in her isolette and hooked up to a CPAP machine that covered most of her face, helping her lungs to take in and put out oxygen. She looked so tiny and helpless, hooked up to machines, with probes on her chest, exhausted from the day’s events of entering this world before she should have. Next, he wheeled me over to the isolette next to hers, to see our son. He too was hooked up to a CPAP machine, with probes on his chest. He looked a little more meaty compared to his sister. Both were still extremely small, tipping the scales at 2lbs 13oz and 3lbs 10oz, respectively. After spending a few hours as a new family in the NICU, we returned to my room to get some rest. When we woke in the morning, we went down to the NICU to see our babies and got to hold them for the first time. What an incredible and indescribable feeling. I cried.

A few hours after those initial snuggles, we received great news-the babies had both stabilized their breathing and were able to come off the CPAP machines. This allowed for skin-to-skin contact to be more comfortable for all of us.

Years of studies have shown the importance of skin-to-skin contact between newborns and parents, especially preemies. Commonly referred to as “kangaroo care,” the loving and patient NICU nurses explained that the most effective and comfortable way to achieve this bonding experience is to slide the baby down into the top of your shirt through the neck hole. Because I was wearing a nursing tank top, I was able to slip my little babes right down onto my chest and have them securely nestled against my skin. Hubby comfortably fit the babies into the v-neck of his undershirt. This was a whole new life for us. We had to learn how to properly care for preemies. We both treaded lightly, because we felt that they were so delicate and fragile. We watched how the nurses handled the babies and soon learned the ropes.
We took each day at a time, having no expectations, but just going with the flow. We celebrated every mL consumed during a bottle feed and every single “inchstone” each baby achieved. We learned how to decipher their cries and satiate their needs. Their distinct personalities emerged immediately, which provided for the rare moments of laughter. Never in my life did I ever expect to be so excited over the contents and weight of a diaper. We learned about heart rate decelerations, apnea episodes, oxygen output levels, how to read the pulse oximeter machine, how to gavage feed, how to bathe our babies, and most importantly, we learned the virtue of patience.
Our son, the bigger of the two babies, progressed more rapidly than our daughter. He was completely healthy and just needed to feed and grow. He took off as soon as he was born, gaining weight and growing each day. By the third week in the NICU, he had reached the minimum weight required for discharge, pending the successful passage of a car seat test. Babies who are nearing discharge must successfully sit strapped into their car seat for one hour without any heart rate decelerations or apnea episodes. He passed with flying colors. Suddenly we were struck with the bittersweet tearing of our hearts: being able to take one baby home while the other baby remained rather sick and indefinitely in the NICU.
The following five weeks tugged on our hearts. It doesn’t get easier to leave a baby behind in the NICU, especially when you have one at home.
I put on blinders and remained focused on getting our baby girl healthy, one day at a time. I stuck to a routine of visiting her every morning at 8am for her feed and to meet with the doctor when he made his usual rounds. I brought her twin brother with me every time we went to visit, and kept the babies as close to each other as possible to provide them comfort and solace. I returned at 1pm and 4pm for her feeds and for snuggles. My mom would usually visit for the 11am or 1pm feeds, and my dad would drop in whenever he had a free moment, as he worked in the hospital. Hubby would drop in after work for the evening feeds and to have private bonding time. Nights were regimented, as I was up every three hours to feed our son and then pump so that I could bring milk to the NICU each day for our daughter. Exhaustion didn’t enter my vocabulary at this stage; I was running on autopilot, focused on the health of our babies.
During the time that our daughter was in the NICU, she continued to experience apnea episodes, also referred to as breath-holding spells. Commonly with preemies, when they are in pain, they hold their breath until they stop breathing. It’s a scary episode and you must stimulate them to get them back. Luckily, when they are in the NICU and hooked up to monitors, the nurses and doctors are nearby to monitor the situation and intervene if the baby doesn’t resolve on their own. Our daughter was quite sick. She had been growth-restricted in-utero, and was born with severe reflux and gastroesophageal reflux disease (GERD). Her digestive system was underdeveloped and she did not have the muscles or coordination to suck, swallow, and breathe. Every single feed was extremely painful for her. She was jaundiced and required intervention and assistance.

At one point, she required a blood transfusion. We had a 7-day stretch with no apnea episodes, but she still wasn’t able to take all 8 daily bottles without a major struggle or having to gavage the remainder into her feeding tube. She was discharged from the hospital and we brought her home to my parents’ house, where we had been living since I gave birth.
We were extremely vigilant and cautious with her when she came home. I followed the NICU schedule and fed her every three hours around the clock, with her twin brother. Everything was going well and we were preparing to pack up and return to our own home for the first time as a family of four. I was taking trips back and forth to the car to load our belongings while the babies napped in the kitchen. Our daughter was sleeping in the swing and our son was sleeping in a Moses basket. As I made a trip into the kitchen past the swing, I glanced down at her to make sure she was still doing ok. Her pallor looked off to me. I held my finger under her nose to feel for her exhaled breath. I didn’t feel anything. I immediately picked her up and tried to summon her awake. Nothing. I laid her on the counter and prepared to begin CPR. She flinched. I raced her upstairs to where my dad was and he helped me stimulate her to bring her back. After we stabilized her, we called the NICU and they told us to bring her back immediately. Our NICU typically doesn’t allow graduates to return to the NICU out of an abundance of caution to not introduce outside germs into the unit that could jeopardize the other babies. But since our daughter had only been released less than 48 hours prior and it was RSV season, they didn’t want her to be on the pediatric ICU (PICU) floor and exposed to a whole host of dangerous germs, so they made an exception.
As soon as we brought her back to the NICU, they did a chest x-ray, gave her a shot of antibiotics, and put her in isolation away from other babies in the unit. This was protocol since she had been outside of the unit and reentered. We spent the next nine days back in the NICU, constantly monitoring her and restarting the clock because she had another apnea episode while in the unit. The NICU’s typical rule is 7 days brady free-which means no apnea episodes or bradycardias where her heart rate or oxygen levels would drop. We hit the 7 day mark and I wasn’t as excited as one would expect. I felt more comfortable having her in the NICU, knowing that she was hooked up to the monitors and having the nurses nearby to intervene if necessary. We spoke to the neonatologist and arranged for our insurance company to provide round-the-clock skilled nursing care for our daughter in our home. Our insurance company also provided us with a pulse oximeter to use at home. With those safeguards in place, we felt more comfortable bringing her home to end this chapter of our lives and begin our happily ever after.
In the following weeks and months, we adjusted to life with preemie twins. Our daughter continued to have a few more apnea episodes, but because she was hooked up to the monitor and the nurse was within arm’s reach, we knew how to handle the situation and take proper care of her. Sleep was a distant memory, but our focus on the health of our babies consumed our days, nights, hours and minutes. We hibernated all winter and reemerged in the spring when the babies were healthier and the risk of RSV had diminished.
© Copyright 2018 Twinstant Gratification, LLC
Tamar Blazer is an attorney-turned-twin mom, with a passion for her family, friends, writing, good food, home decor and laughing. When she’s not lamenting on her lack of sleep, you can find her doing one of the too many projects she likes to take on, usually with a twin on either side.









Our stories are so similar, from preterm delivery, to apnea, to pulse-ox use at home. The NICU experience is always one to remember. The ups, downs, highs and lows. It’s an emotional roller coaster. Something amazing though, is how once my girls were home, the NICU stay became a distant memory, overcome by the hectic life of a newbie twin mom.